Antibiotic Resistance
The Dichotomy of Access, Innovation & Sustainable Use
Antibiotic Resistance
The Dichotomy of Access, Innovation & Sustainable Use
Transcript of talk delivered by Mr. Saransh Chaudhary (CEO of VMRC) at Manthan 2018
Good evening Ladies and Gentlemen,
It is a great honor and privilege for me to be here today and speaking in front of such distinguished audience. It is also an honor to represent my company, Venus Remedies Limited and Venus Medicine Research Centre, here in Chandigarh, where the foundation was laid down about 27 odd years ago.
My topic for discussion today, obviously is AMR, but not just the societal problem of this global catastrophe ahead of us, but also about what got us here and what can perhaps get us out of it.
The upcoming antibiotic pipeline is almost dry, and even the drugs that are currently under development, palpable challenges need to be overcome before these new drugs can eventually be used in clinical settings.
In my view, AMR is more of a global public health hazard than a regional crisis that will eventually subside. In the panel discussion, we have already heard about the critical situation as it stands in various parts of the country, so I would like to talk about what in fact got us here.
This is the antibiotic timeline, where the red line indicates the need for antibiotics over the past century and what the future would perhaps look like. The grey line on the other hand indicates the availability of antibiotics over the same time period. Now clearly, in the pre-antibiotic era, the need for effective antimicrobials was at an all-time high, given that no effective alternative existed to treat even the simplest of infections. But then in 1943, with the advent of penicillin, a whole new era for medicine began. But humans almost immediately overexploited this wonder cure and in the latter part of the 20th century, the availability of antibiotics was far greater than was needed at the time. This led to the emergence of resistance in the bacterial species, marking the onset of the crisis that we face today.
In the pre-antibiotic era, the need was greater than access and so it drove innovation. During the golden years as some call it, or the latter of the 20th century, productivity was the main goal for the industry and that led to the rapid emergence of resistant bacteria. Now we stand in times where the need for new antibiotics is almost at an all-time high, but unfortunately, there aren't nearly as many companies doing antibiotic research as is needed. We stand at the inflection point where we have the power to bridge this gap between need and availability and in turn control the spread of resistance for a more sustainable future.
Here I mention that in the future, the need for new antibiotics is greater than the opportunity. Here is what I mean by that:
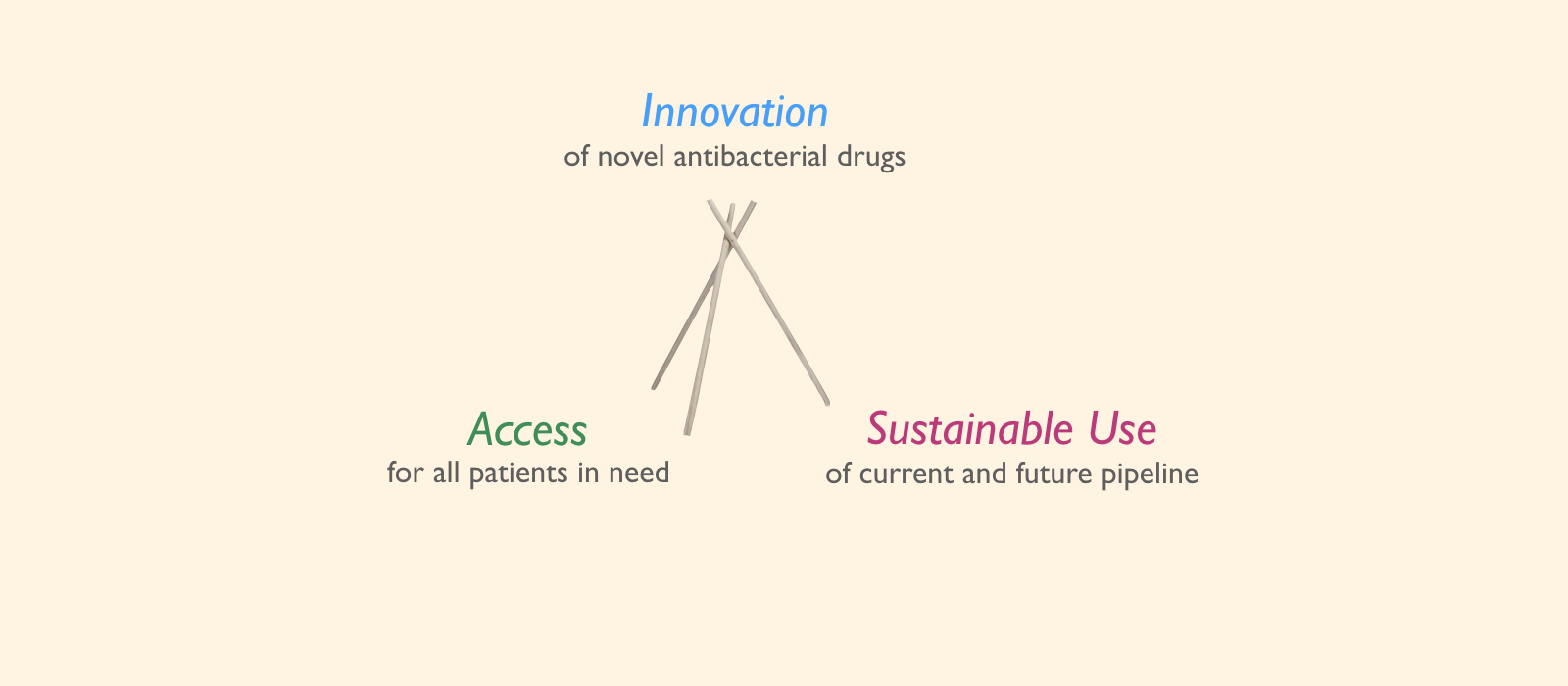
The current ecosystem of anti-infectives, especially antibiotics, can be summed up in this slide. We call it the Antibiotic Tripod. Firstly, we want INNOVATION of novel antibacterial drugs, then we would want that ACCESS of these drugs should be to all patients who need them and lastly, we want that these drugs and existing drugs are used sustainably so that we don't speed resistance. Now some of you may have identified the dichotomy of the situation here, but clearly all three aren't simple to achieve. Here's why!
Innovation without Access if Unjust to the companies because the economics just don't add up and also to the patient because they may be deprived of the right treatment while it exists.
On the other hand, Innovation without Sustainable Use is Wasteful because it would undermine the very problem at hand.
The same way, Access without Sustainable Use would spread resistance. And although we want it, but Sustainable Use constrains Access and Undermines innovation.
So just like this tripod here, we need a balance of these three things, but is this really achievable?
Well from the industry's perspective, antibiotics are no longer profitable. Here are some statistics to support that cause:
Adhering to the guidelines, specifically t font-size:14px;alk about clinical trials as we are here to discuss that today, there are four significant challenges:
- EMA/FDA manufacturing facilities are required
- Clinical Trials need to be of a double-blind design to bring in relevant statistical evidence
- Only one indication can be tested in one study protocol, barring a few exceptions
- And the choice of comparator group makes it increasingly difficult to reproduce the desirable evidence
As a result of such strict and rapidly changing regulatory environments, this is what has happened:
The expectation from the industry is far greater than what is economically feasible. Given that antibiotics treat acute infections for which therapy only last for days, the sales of the new antibiotics in the past decade compared to other therapy areas is meagre.
The review on AMR highlighted that companies will only make profit in the 23rd year of investment, but if we also factor in for sustainable use, that may also never happen. And mind me but I am not advocating for the injudicious use of antibiotics in any way, I am just trying to highlight the facts as they stand, and the fact is that Risk is too high, while the Rewards are too low.
Now fortunately for us, this problem has also already been identified by certain groups and put forward at global stages. The results of these efforts can be seen on this slide. This slide consists of groups, initiatives, charities and statutes that have all arisen as a response to cater to the growing disinvestment in antibiotics.
Although various initiatives have been discussed, one is particularly interesting. This is the de-linkage of R&D with the price of medicine, or in fact the reimbursement of the investment. A floating idea is that governments should step forward and reimburse companies for their R&D effort and in return they would take over the pricing, distribution and positioning of these new drugs to ensure their sustainable use.
This model was first proposed by the civil societies as a better way of financing R&D than the patent-based system, but heavily opposed by the industry as it was considered a challenge to the free market and companies voiced their disapproval on govts deciding on how to reward R&D. Well in the light of the recent economics, this solution may not be unfeasible anymore. Well, I may not agree with it completely but at least it is a step in the right direction.
In my view, the entire ecosystem needs to come together and work in synergy, and that is the only way forward.
At Venus, our approach towards saving antibiotics is slightly different. We believe in preserving the efficacy of existing antibiotics as new ones can only do so much. We identified a middle ground with Antibiotic Resistance Breakers. We strongly believe that ARBs can bring about a tangible societal impact, while being more economically feasible. Therefore, for the past 15 years, VMRC has been committed in its effort and today it is a landmark occasion as we unveil the results of the plea clinical trial as part of an ongoing endeavor to solve the antibiotic resistance crisis. Thank you!
Latest Posts
Social Responsibility
Talk to Us
Our Presence
© All Rights Reserved | Privacy Policy | Adverse Drug Reaction
Antibiotic Resistance